Updates and articles about Bariatric Procedures
 Bariatric Surgery FAQs with Dr. Abbas
Bariatric Surgery FAQs with Dr. Abbas
 Can the Gastric Sleeve be Performed on an Outpatient Basis?
Can the Gastric Sleeve be Performed on an Outpatient Basis?
 Are You at Risk of Diabetes?
Are You at Risk of Diabetes?
 Can Thinning the Waist Help Prevent Thinning in the Brain?
Can Thinning the Waist Help Prevent Thinning in the Brain?
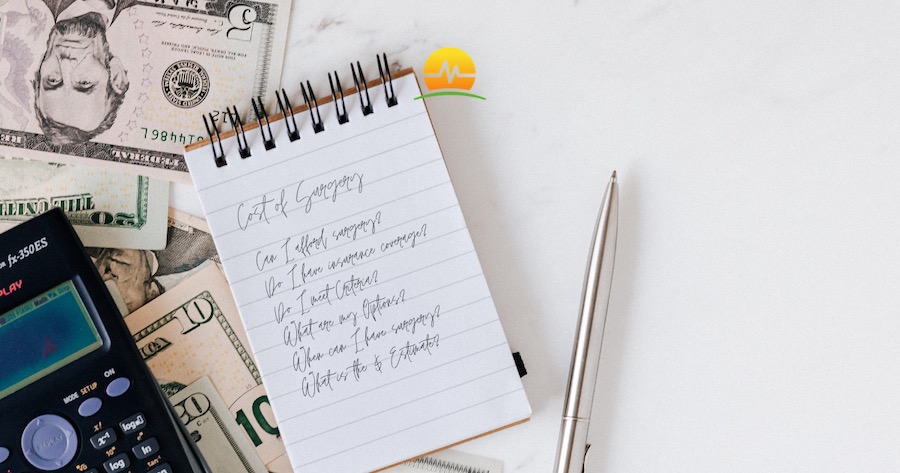 Understanding Your Bariatric Surgery Insurance Coverage
Understanding Your Bariatric Surgery Insurance Coverage
 Understanding Dumping Syndrome
Understanding Dumping Syndrome
 Will I Lose Weight after Bariatric Surgery?
Will I Lose Weight after Bariatric Surgery?
 Cutting Through the Weight Loss Hype
Cutting Through the Weight Loss Hype
After Weight Loss Surgery
Bariatric Procedures
Bariatric Surgery
BMI
Colonoscopy
Colorectal Disease
COVID-19
Diabetes
Diet
Diverticulosis
Exercise
Expectations
Gallbladder Surgery
Gastric Bypass
Gastric Sleeve
General Surgery
GERD
Getting Started
Hemorrhoids
Hernia Surgery
Hydration
In The News
Joints
Obesity
Osteoarthritis
PPIs
Premier Protein Recipes
Robotic Surgery
Sleep
Social Media
Support
Wegovy/Zepbound
Weight Loss
Weight Loss 101