You notice a little blood when you wipe, maybe some discomfort during bowel movements, and suddenly your mind leaps to the worst-case scenario – colon cancer.
Realistically, most rectal bleeding isn’t cancer. More often than not, it’s caused by something far less sinister, like hemorrhoids or anal fissures. Still, distinguishing the benign from the potentially serious is important and can be life-saving.
Paying attention to your bowel patterns may not be the highlight of your day, but noticing changes in stool color, consistency, or frequency can provide valuable clues about your digestive health. Early awareness allows you to address minor issues before they escalate and ensures that anything more serious is caught promptly.
Even small, seemingly insignificant changes can be early warning signs, giving your healthcare team a head start in diagnosing potential problems and keeping your digestive system on track.
Hemorrhoids: The Common Culprit
Hemorrhoids are swollen veins in or around the anus that can cause discomfort, itching, and bleeding. They’re extremely common, affecting roughly 5% of Americans, with prevalence increasing with age – about half of adults over 50 experience them.1 They can be internal (inside the rectum) or external (around the anus) and often appear with:
- Bright red blood on toilet paper or in the toilet
- Itching, irritation, or a feeling of localized “fullness”
- Swelling or a palpable lump near the anus
- Discomfort or pain, especially with external hemorrhoids
Hemorrhoids often flare up due to straining during bowel movements, pregnancy, chronic constipation, or prolonged sitting. Most are harmless and can be managed with lifestyle changes (like increasing fiber and fluids and avoiding straining), over-the-counter creams, or minimally invasive procedures. Maintaining a high-fiber diet, staying hydrated, and getting regular exercise are preventive measures that can significantly reduce the frequency and severity of flare-ups.
Anal Fissures: Small But Painful
Anal fissures are small tears in the lining of the anus, often caused by passing hard stools or chronic diarrhea. While they may seem minor, fissures can be intensely painful and linger if not addressed.
Unlike hemorrhoids, which are swollen veins, fissures are actual splits in the skin or mucosa. This difference explains why fissures often produce a sharp, tearing pain during bowel movements, sometimes accompanied by bright red blood.
Common features of anal fissures include:
- Sharp pain during or immediately after bowel movements
- Blood streaks on stool or toilet paper
- A visible crack, small lump, or skin tag on the skin around the anus, especially in chronic cases
- Possible spasm of the anal sphincter, making bowel movements even more painful
Like hemorrhoids, fissures are typically benign and respond well to fiber, hydration, and topical treatments, and often heal on their own with proper stool softening and sitz baths. Chronic or recurring fissures may require prescription ointments, Botox injections, or minor surgery to alleviate symptoms.2
Colon Cancer: What Sets It Apart
Colon cancer, on the other hand, may present subtly, but can also mimic benign conditions. It arises from abnormal growths, or polyps, in the colon or rectum that can become malignant over time. Unlike hemorrhoids or fissures, colon cancer can silently progress without obvious discomfort until it reaches an advanced stage.
Warning signs may (but not always) include:
- Persistent or unexplained changes in bowel habits, like diarrhea, constipation, or narrowing of the stool
- Blood in the stool (often darker or mixed throughout the stool rather than streaked)
- Unexplained fatigue or weakness
- Unintentional weight loss
- Abdominal pain, cramping, bloating, or a feeling of incomplete evacuation
Unlike hemorrhoids or fissures, colon cancer does not resolve on its own. Early detection dramatically improves outcomes, making awareness and screening crucial, especially since nearly 4 out of every 100 people will be diagnosed with colorectal cancer at some point in their lives.3
Certain risk factors can increase the likelihood of developing colon cancer. Age is a significant factor, with most cases occurring in people over 45, though rates in younger adults are rising. A family history of colorectal cancer or polyps, inflammatory bowel disease (such as ulcerative colitis or Crohn’s), and genetic syndromes like Lynch syndrome all heighten risk.
Lifestyle factors (such as a diet low in fiber, high in red or processed meats, obesity, smoking, and heavy alcohol use) also play a role. Understanding these risk factors can help guide lifestyle changes, screening schedules, and discussions with your healthcare provider.
Screening through colonoscopy or stool-based tests at recommended intervals starting at age 45 are the best tools currently available for detection. Colonoscopy is the gold standard for discovering colon cancer or even preventing it by removing polyps before they become malignant. For those at higher risk, screening can begin as early as age 30 because early-stage colon cancer often produces no symptoms. Catching precancerous changes early can save your life.
When to See a Doctor
Rectal bleeding, pain, or changes in bowel habits are never something to ignore. While hemorrhoids and fissures are common culprits, only a healthcare professional can determine the underlying cause and rule out more serious conditions.
Seek medical attention if you notice:
- Persistent or unexplained rectal bleeding, especially if it is heavy and/or mixed with stool
- Dark, tar-like, or blood-streaked stool
- Changes in bowel habits lasting more than a few weeks
- Unexplained abdominal pain, weight loss, or fatigue
- Lumps or swelling that don’t resolve
- Any other concerning or abnormal bowel symptoms
Early evaluation leads to proper diagnosis and treatment. Even if it turns out to be a hemorrhoid or fissure, your doctor can help manage symptoms and rule out anything more serious. Hemorrhoids or fissures may require lifestyle adjustments, topical medications, or minor procedures, while colon cancer caught early can be treated successfully with surgery, chemotherapy, or other targeted therapies.
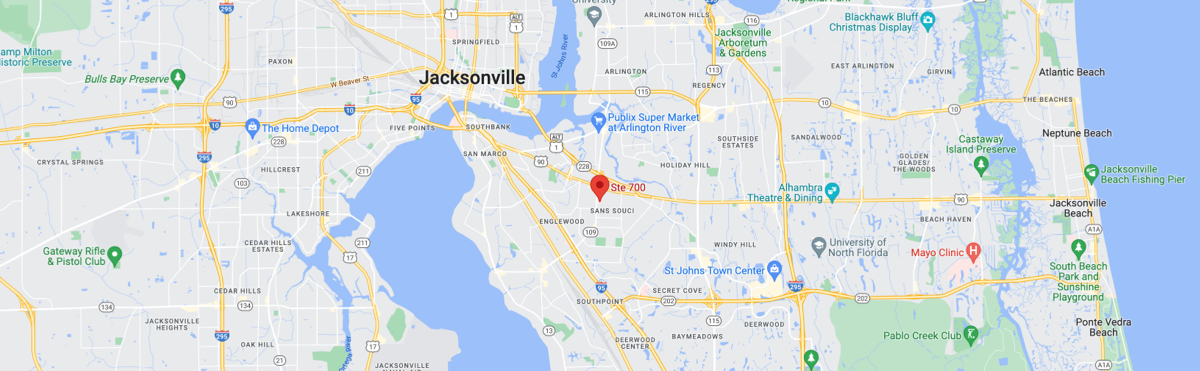
At MASJax Bariatric and General Surgery, our team provides compassionate, thorough care for patients experiencing rectal bleeding or other gastrointestinal concerns.
Led by board-certified general surgeons and fellowship-trained colon and rectal surgeons Dr. Alex Crean and Dr. Andrew Schlussel, we offer advanced screening and diagnostic tools to distinguish between common conditions, such as hemorrhoids and fissures, and more serious diseases.
Don’t wait – schedule a consultation today for personalized care and peace of mind.
- NIH National Institute of Diabetes and Digestive and Kidney Diseases. (2016, October). Definition & Facts of Hemorrhoids – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/definition-facts#common.
- Thippeswamy, K. M., Gruber, M., Abdelaziz, H., & Abdel-Dayem, M. (2025). Efficacy and safety of botulinum toxin injection in the management of chronic symptomatic anal fissure: a systematic review and meta-analysis of randomized controlled trials. Techniques in coloproctology, 29(1), 44. https://doi.org/10.1007/s10151-024-03087-y.
- National Cancer Institute. (2025). Cancer Stat Facts: Colorectal Cancer. National Cancer Institute. https://seer.cancer.gov/statfacts/html/colorect.html.