Updated for 2023!
We all experience sore or itchy rear ends at some point in our lives, often resolving with proper self-care. Some of us may even experience painful bowel movements and bright red streaks of blood in the toilet. This is a common reason to visit a colorectal surgeon like Dr. Alex Crean at MASJax. Fortunately, most cases of bright red blood during a bowel movement and resultant discomfort or pain are caused by a benign condition known as hemorrhoids or piles. However, this condition can be easily confused with anal fissures – small cuts or tears in the lining of the anus. How can you tell the difference? With similar symptoms, it can be difficult for patients to figure out what’s happening, and blood presence is downright frightening. Don’t even get us started on Dr. Google; that can easily convince a worried patient. An exam by a trained colorectal physician will help you to get a precise diagnosis of your condition and find the best treatment for you sooner rather than later.
Hemorrhoids 101
If you are experiencing painful passing of stool and noticing bright red blood during your bowel movements, you likely have hemorrhoids. While hemorrhoids can be painful and irritating, the good news is that they aren’t likely to cause long-term damage, though they can be very uncomfortable.
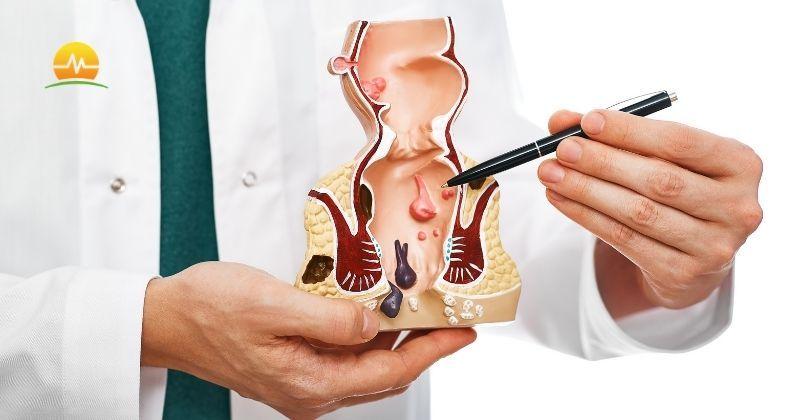
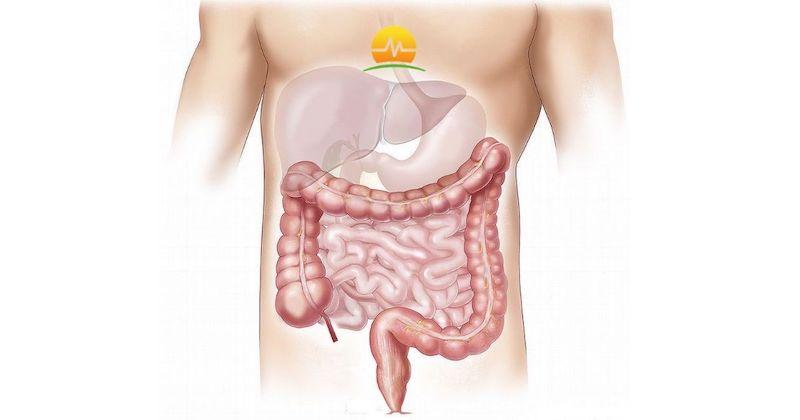
Hemorrhoids are a common condition, affecting about three-quarters of us by age 50. They are often associated with straining during bowel movements, commonly due to chronic constipation or diarrhea. Sitting for extended periods on the toilet also interferes with normal blood flow. This straining or interference in blood flow can cause blood to pool in the blood vessels, creating a varicose vein in the anus. Hemorrhoids also commonly occur in pregnant women due to pressure from the growing child and increased blood flow to the area.
While some hemorrhoids are asymptomatic, people with hemorrhoids often experience anal pain, bleeding, itching, or notice a lump or protrusion from the anus. Hemorrhoids may also come with unpleasant anal leakage of stool or mucus. Hemorrhoids are typically a condition we want to treat soon to get patients back to a more comfortable everyday life.
A particularly painful condition occurs when the hemorrhoidal vein develops a clot or thrombosed hemorrhoid, and this is not dangerous but can cause significant pain. If left untreated, a thrombosed vein can ulcerate and cause bleeding.
Treatment for hemorrhoids can range from topical ointments and suppositories found over the counter to in-office therapy and outpatient surgery, including a hemorrhoidectomy. Smaller hemorrhoids may go away on their own.
We understand that there could be an element of anxiety or embarrassment related to evaluating hemorrhoidal disease. It is important to realize that every one of us has hemorrhoids to some degree. We are all born with them, as hemorrhoids represent a portion of the natural mechanism we have to help control our bowel movements.
Anal Fissures Explained
Anal fissures are relatively common, with over 250,000 diagnosed yearly in the US. You can imagine that many more cases are treated at home. Anal fissures occur when there is a split or tear in the thin skin of the anus. This can happen from a particularly hard or large bowel movement, and most patients will recall this event happening shortly before the onset of symptoms, maybe within a few days. An anal fissure can also result from trauma to the anus, including scratching. These cuts are common, and usually, patients recognize symptoms, including severe pain and bleeding with bowel movements.
Anal fissures will be classified as acute, lasting less than six weeks, or chronic, based on how long a patient has been experiencing symptoms, and treatment varies accordingly. For some, anal fissures can be challenging to heal due to the normal, active use of the anal sphincter causing frequent wound reopening. Luckily, treatments have been developed with this in mind, including temporarily paralyzing the muscle.
Your physician or colorectal surgeon should direct any treatment for anal fissures. Once we have diagnosed an anal fissure, the initial management includes topical ointments that help to relax the sphincter muscle and allow the tear or fissure to heal. The commonly used ointments are topical diltiazem, nifedipine, or nitroglycerin. We typically use diltiazem or nifedipine first. Nitroglycerin is also very effective but can carry a side effect of significant headaches. Lifestyle modifications can also help by increasing your daily water intake and starting a bowel regimen to include stool softeners or laxatives. In our practice, we will help to tailor an appropriate bowel regimen to your daily bowel function and lifestyle.
Procedural intervention is typically recommended if your symptoms do not respond to topical ointments. The most effective treatment for chronic anal fissures is a lateral internal sphincterotomy with fissurectomy. This involves surgically removing the inflamed fissure tissue and making a small cut within the sphincter muscle to break the spasm cycle and allow the fissure to heal. This is a highly effective treatment with excellent long-term response rates. If patients would like to avoid the small cut in the sphincter muscle, another treatment option offered at our practice is administering Botox into the sphincter muscle to allow for temporary relaxation/paralysis to heal the fissure. We aim to work with our patients to choose a treatment plan that best suits their lifestyle.
Evaluation
An experienced colorectal specialist like Dr. Crean knows that patients are often in pain when they see him. Our goal is always to offer the fastest, most effective treatments for hemorrhoids or anal fissures. You will start by discussing your symptoms and medical history, and our team will evaluate any risk factors you may have that make one condition more likely than the other. Sometimes a determination can be made without an invasive exam. Otherwise, a digital rectal exam will be needed. We aim to make a definitive diagnosis while minimizing pain or discomfort.
Be Proactive
Most patients can take simple steps to prevent hemorrhoids and anal fissures from occurring or reoccurring. These steps are generally good for your bowel health and can include the following:
- Incorporating fiber into the diet. This can be done through food choices or with a daily fiber supplement (gummy, tablet, or powder). Healthy, high-fiber diets add bulk to bowel movements, making them move more quickly through the intestine with less time to become impacted.
- Stay hydrated. Drinking water and maintaining good hydration will also aid in passing healthier stools. The colon absorbs water to make it easier to eliminate stool. Staying adequately hydrated creates bulk but soft stools that are passed easily.
- Make exercise a priority. Exercising helps with bowel health along with improved overall health.
- Do not sit on the toilet for too long. Dr. Crean suggests that electronic devices are not used as they prolong the time you sit.
- Speak to your doctor about stool-softening medications or suppositories. And give your doctor a list of medications and supplements you may be taking, as some may cause hard stools or constipation.
- Enjoy a warm bath, known as a sitz bath, which can relieve pain and itching while also soothing the skin.
- Speak to your doctor about what kind of toilet paper to use. Or if you should use moist or medicated wipes.
- Go to the toilet as you would normally. While you may be worried about the pain associated with hemorrhoids or anal fissures, you will undoubtedly make it worse if you become constipated.
- How you use a toilet may also make a difference. Modern toilets that keep our upper bodies at a 90° angle to our lower body can create a “kink” that makes passing a bowel movement harder. Patients would be well served to sit on the toilet in a squatting position, and this is most easily achieved using a stepstool to raise the feet off the ground by a foot or 18 inches.
Could It Be Colorectal Cancer?
Anal fissures and hemorrhoids have many symptoms in common with anorectal and colon cancer. Only your colorectal specialist can offer a proper diagnosis one way or the other, but you’ll be happy to know that hemorrhoids and anal fissures do not cause cancer, nor are they a sign of cancer, though they can cooccur. If your symptoms do not abate with treatment or you begin to feel worsened discomfort, you should visit your colorectal surgeon for further diagnosis. Also, remember to get your colonoscopy at the appropriate interval discussed with your doctor.
Next Steps
We encourage you to schedule an appointment with Dr. Crean if you are experiencing uncomfortable symptoms of hemorrhoids or anal fissures. Our goal is to address your concerns and symptoms professionally and efficiently, and our philosophy for treatment is achieving excellent symptomatic control with the smallest amount of procedural intervention possible. Because symptoms of both conditions can be similar to other, more colorectal severe diseases, your doctor may want additional testing performed to rule out anything beyond what can be treated in the office. It is essential not to ignore symptoms or suffer when you don’t have to.